Your Guide to NDIS Medication Chart Compliance
An NDIS medication chart is the go-to document for safely managing and keeping track of a participant's medications. Think of it as the central nervous system for their health support – it’s a critical tool for support workers to ensure the right person gets the right dose at the right time, every single time. It’s what stands between quality care and dangerous errors.
Why a Perfect NDIS Medication Chart Is Non-Negotiable

A well-kept NDIS medication chart goes way beyond just ticking a compliance box. In reality, it’s the backbone of safe and effective participant support. This isn’t just paperwork; it’s a non-negotiable tool for upholding a person’s dignity, fostering their independence, and guaranteeing consistent care, no matter who is on shift. It acts as the single source of truth for support workers, family members, and allied health professionals alike.
Let's put this into a real-world context. Imagine a participant with a complex routine, taking medications for epilepsy, high blood pressure, and chronic pain. A new support worker comes in for their first shift. Without a crystal-clear, up-to-date chart, the risk of misinterpreting instructions is huge. A missed anti-seizure dose or giving pain relief at the wrong time could have serious consequences. A precise chart eliminates that guesswork.
Preventing Errors and Upholding Safety
The stakes are incredibly high when it comes to medication management. An inaccurate or disorganised chart can easily lead to:
- Adverse drug interactions if all medications aren’t documented in one place.
- Incorrect dosages, which can be ineffective or, even worse, toxic.
- Missed doses, which can seriously compromise a participant’s health and stability.
The sheer volume of medication use in Australia puts this into perspective. We know that nearly seven in ten people have been dispensed at least one medication. For Australians aged 75 and over, that number skyrockets, with 32.6% receiving ten or more different types of medication. With so many people managing multiple prescriptions, a reliable NDIS medication chart isn't just helpful—it's absolutely essential.
A medication chart is far more than a simple list. It’s a vital communication tool that connects different support workers across various shifts and bridges the gap with other healthcare providers. It ensures everyone involved in a participant's care is on the same page.
This level of meticulous documentation is a fundamental part of a participant's overall support strategy. It needs to be treated with the same level of care as their NDIS plan itself and should be reviewed regularly, just like the process we detail in our guide to a successful NDIS plan review.
To truly appreciate why a perfect chart matters so much, it’s useful to look at the bigger picture, like the importance of accurate information in healthcare. This principle highlights just how critical precision is in every single medical process. At the end of the day, this document isn’t just about administrative tasks—it’s about safeguarding a person’s health and honouring the deep trust they place in their support team.
Gathering the Right Information Before You Start

It’s easy to jump straight to finding a template, but a truly effective NDIS medication chart starts long before that. The real foundation is built on accurate, comprehensive information.
Skipping this prep work is a bit like trying to build a house without a blueprint—it might stand for a little while, but it’s bound to have problems. Taking the time to collect every detail upfront prevents confusion and, most importantly, reduces the risk of dangerous medication errors down the track.
The aim here is to create a single, reliable source of truth that anyone involved in the participant's care can understand at a glance. This is crucial for smooth handovers between support workers or when new team members come on board.
Participant and Medical Team Details
First things first, let's get the basics down. This isn't just about filling in boxes; this information is often the first thing someone needs in an emergency.
Make sure every detail is current and clearly written.
- Participant’s Full Name and Date of Birth: Double-check the spelling and details are correct.
- Primary Contact Person: Include their name, relationship to the participant, and a reliable phone number.
- GP and Specialist Information: List the names, clinics, and phone numbers for every healthcare professional involved.
- Pharmacy Details: Note the preferred pharmacy’s name, address, and contact number. This makes chasing up scripts and refills so much easier.
This information is a core part of a participant's broader support framework, tying directly into their primary care plans. It all works together. For more on how these documents connect, take a look at our guide to your NDIS service agreement.
Comprehensive Medication List
Now for the most critical part: the medication specifics. There's no room for guesswork here; precision is everything.
You should always consult directly with the participant's GP or pharmacist to verify every single item. You'll need the exact medication name (both brand and generic, if you can get it), the prescribed dosage (e.g., 50mg, not just "one tablet"), and the route of administration (e.g., oral, topical, inhaler).
Don't forget to include those small but vital instructions that can affect how well a medication works or how safe it is, like "take with a full glass of water" or "must be taken with food."
By standardising the information you collect, you create a consistent, legible, and accurate record for everyone. This principle is fundamental to preventing medication errors and ensuring participant safety.
This isn't a new idea. It mirrors the approach taken in hospitals across Australia. The creation of the National Inpatient Medication Chart was a huge step forward in reducing errors simply by standardising how prescription information was recorded. You can read up on the history behind these national charts and see how the core principles apply directly to creating a safe and effective NDIS medication chart.
Lastly, make sure you document any known allergies, potential side effects to watch out for, and crystal-clear instructions for any PRN (as-needed) medications. Having this complete picture empowers support workers to provide care that is confident, safe, and truly person-centred.
Choosing and Customising Your Chart Template
Alright, you’ve gathered all the essential information. Now comes the practical part: deciding on the format for your NDIS medication chart. You’re essentially looking at two main paths: the trusty, traditional paper chart or a more modern digital app.
There’s no single "best" answer here. The right choice really hinges on the participant's specific needs, their living situation, and how comfortable the support team is with technology.
Paper vs. Digital: What’s the Right Fit?
For many, paper charts are the go-to. They’re simple, don’t need an internet connection, and can be physically present where they’re needed most—stuck on the fridge or in a dedicated binder. This high visibility means they’re always accessible to support workers. The downside? They can get lost or damaged, and every little change requires a manual update, which can get messy and time-consuming.
On the other hand, digital apps offer some slick advantages. You get things like automated reminders, the ability for the whole team to see updates in real-time, and a much tidier record-keeping system. But they come with their own challenges. They’re useless without a charged device and a stable internet connection, and everyone on the team needs to be properly trained to use the software.
This simple workflow visualises the core process of using any NDIS medication chart, whether it’s on a screen or on paper.
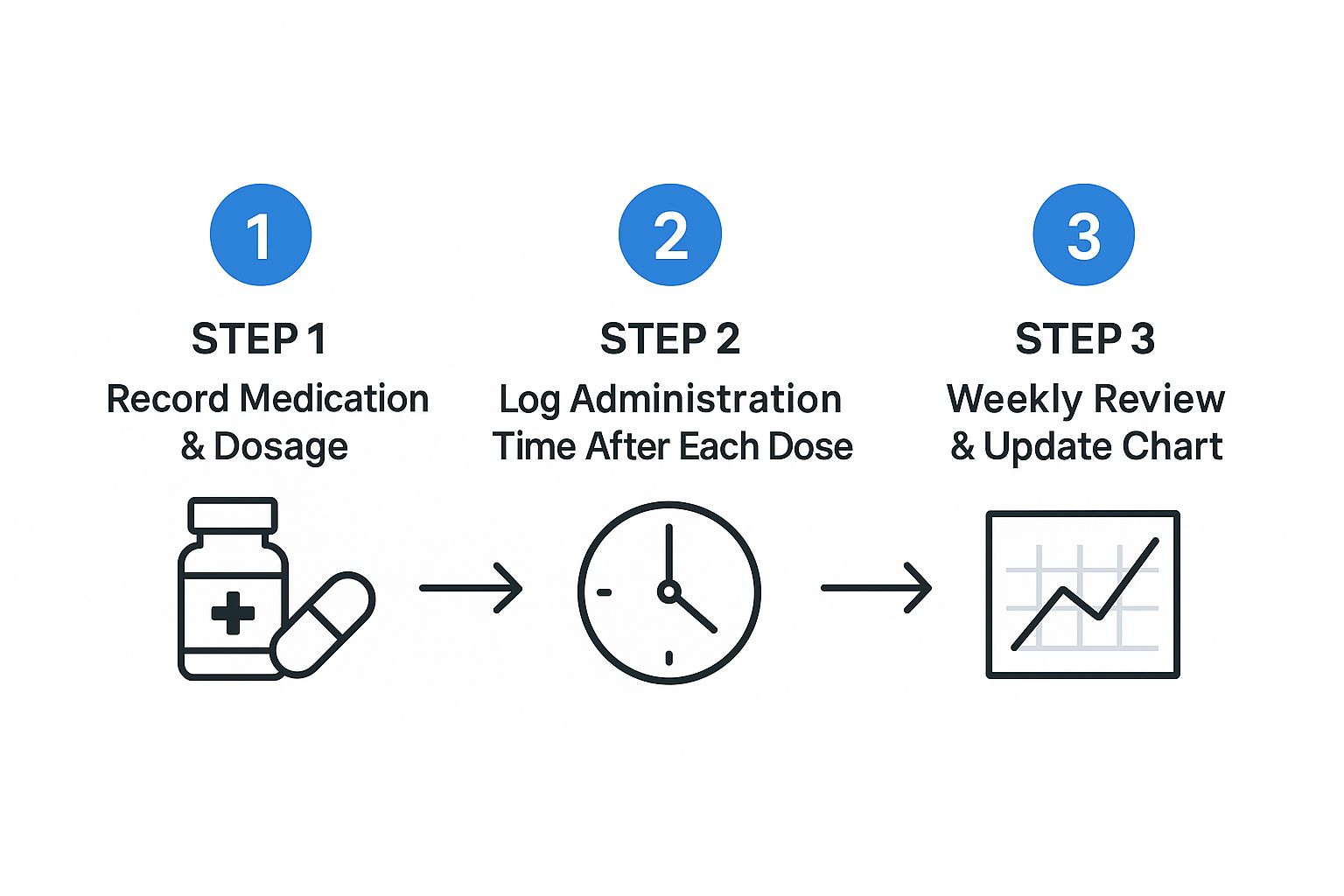
This cycle of recording, logging, and reviewing is constant. It's the key to keeping medication administration safe and consistently accurate.
Digital vs Paper NDIS Medication Chart
To help you weigh the options, here's a quick comparison of what you can expect from each format.
| Feature | Digital Chart (App) | Paper Chart (Printable) |
|---|---|---|
| Accessibility | Requires a smart device and internet. Can be accessed remotely. | Physically present on-site. No technology needed. |
| Updating Information | Instantaneous updates shared with the entire team. | Requires manual changes; old versions must be destroyed. |
| Record Keeping & Auditing | Clean, searchable, time-stamped logs. Easy to generate reports. | Can be messy, prone to handwriting errors, harder to audit. |
| Reminders | Automated push notifications and alerts for scheduled doses. | Relies on manual systems (e.g., alarms, team communication). |
| Security & Durability | Secure data storage (cloud-based), but vulnerable to tech failure. | Prone to physical damage (spills, loss), but not system crashes. |
| Ease of Use | Can have a learning curve; requires tech comfort. | Intuitive and straightforward for most users. |
Ultimately, the decision comes down to your specific operational needs and the preferences of the participant and their support team.
Getting Your Template NDIS-Compliant
Whether you go with an app or a printable template, simply downloading something generic off the internet won't cut it. To meet NDIS Quality and Safeguarding standards, you need to customise it. True compliance isn't about ticking a box; it's about creating a practical tool that genuinely supports person-centred care.
Your goal is to make the chart clear, comprehensive, and auditable. It needs to tell the complete story of a participant's medication support.
Here are a few essential customisations you'll need to make:
- A Dedicated Space for Initials: Every single time a medication is given, the support worker must sign or initial the entry. This isn't optional—it creates a clear audit trail and establishes accountability.
- Precise Administration Times: "Morning" is too vague. Add a column to write down the exact time a dose was given, like 8:05 AM. This is absolutely critical for medications that are time-sensitive.
- A Way to Track Refused or Missed Doses: You need a clear system for this. Create a section to document when a participant refuses their medication or if a dose is missed for any reason, with space for notes explaining what happened.
- A Log for Side Effects and Observations: This is so important. Add a section to note any changes you see in the participant after they've had their medication. A simple note like, "Seemed drowsy 30 mins after dose," provides invaluable information for doctors and nurses during reviews.
Think of the medication chart as a legal document, because it is. It has to be crystal clear, legible, and provide a perfectly accurate record of the support provided. Every field you add should be there to remove guesswork and improve safety.
By tailoring your chosen NDIS medication chart with these details, you turn it from a basic checklist into a powerful tool. It becomes a central document in the participant's support plan, making sure everyone on the team has the right information to provide safe, consistent, and high-quality care. It's this level of detail that shows a real commitment to the participant's health and wellbeing.
Training Your Team for Flawless Chart Use

A perfectly designed NDIS medication chart is only half the battle. Its real value comes to life when it’s used accurately and consistently by every single person on the support team. Without proper training, even the best template can fall short, introducing serious risks and undermining a participant's safety.
Integrating the chart into daily routines isn't just about handing over a document; it’s about building a culture of meticulous, person-centred care. Every support worker needs to understand not just what to do, but why each step is so critical.
This is how the chart transforms from a piece of paper into the central, trusted tool for medication management in the participant's support plan.
From Walkthrough to Real-World Scenarios
Good training has to be hands-on. Start by walking your team through the chart, section by section, explaining the purpose of every field. Cover everything from the medication name and dosage to the spaces for initials and notes on side effects.
I’ve always found that using a completed, anonymised chart as a teaching example works wonders. It shows the team what a high-quality record actually looks like. You can point out how to document precise times, what to do when a dose is refused, or how to correctly record a PRN medication. A solid visual example is so much more effective than just talking about it.
Once everyone is familiar with the layout, it's time to test their knowledge with mock scenarios. This is where the theory hits the road.
- The Missed Dose: A participant was asleep when their 8 AM medication was due. How does the team document this, and what’s the protocol for reporting it?
- The Refused Dose: The participant declines their evening medication. What specific notes should be made on the chart, and who needs to be informed?
- The Adverse Reaction: A support worker notices the participant seems unusually dizzy after taking a new medication. How is this observation recorded, and what are the immediate next steps?
Running through these situations in a controlled environment builds confidence and muscle memory. It ensures that when a real issue comes up, your team reacts correctly and consistently, without a second thought.
The heart of flawless chart use is embedding the 'Check, Administer, Document' process. It's a non-negotiable, three-step cycle for every single dose. Check the chart, administer the correct medication, and document it immediately—no exceptions.
Establishing Clear Protocols and Ongoing Checks
Beyond the basics of filling out the chart, your training must cover the protocols for those non-routine events. What happens if a medication runs out unexpectedly? Who is responsible for contacting the pharmacy or GP? Having clear guidelines in place prevents confusion and stress when things don't go to plan. A skilled https://vanacare.com.au/blogs/vana-care-blog-ndis-news-disability-support-insights-for-south-australia/disability-support-coordinator can be invaluable here, helping to establish these higher-level processes and ensuring the whole team is on the same page.
Regular checks and audits are also absolutely vital for maintaining high standards. This isn't just a best practice for NDIS providers; it's a principle mirrored in Australian hospitals, which use audit systems for the National Standard Medication Chart to monitor compliance and drive improvements in medication safety.
By regularly reviewing your own charts, you can spot patterns, address knowledge gaps, and uphold national safety standards. This kind of continuous oversight is what ensures your NDIS medication chart remains a reliable and effective tool for everyone involved.
Keeping Your Medication Chart Accurate and Current
An NDIS medication chart isn't a "set and forget" document. It’s a living record that has to mirror the participant's health journey in real-time. A chart that’s even a few weeks old can be just as dangerous as not having one at all.
This constant upkeep is absolutely vital for safety and ensuring smooth continuity of care. It means every support worker, family member, and visiting health professional is on the same page, working from the most current information and preventing potentially serious mistakes.
Establishing a Clear Review Schedule
To keep the chart razor-sharp, you need to be proactive. Don't wait for something to go wrong. Instead, have clear triggers that automatically prompt a review and update.
A solid review rhythm means checking the document at these key moments:
- After every single GP or specialist visit. Even if nothing was changed, it’s a perfect opportunity to confirm the current regimen is still correct.
- Immediately when a new medication is prescribed, a dosage is adjusted, or a medication is stopped. This has to happen before the next dose is due.
- Following any hospital admission or discharge. Medication lists are almost always changed during these transitions, making this a critical checkpoint.
- At regular quarterly intervals as a standard best practice, even if none of the other triggers have occurred.
Who Needs to Be in the Room
Getting the chart right is a team sport. Whenever possible, a review should involve everyone who has a stake in the participant's health and wellbeing. That starts with the participant themselves—their voice and preferences must always be at the centre of the conversation.
Family members or a primary carer should be there too; they often have priceless insights into daily routines and how the participant is responding to medication. Most importantly, a healthcare provider—like the GP, pharmacist, or a community nurse—should be consulted to verify that all the medical details are spot on. This collaborative approach is the best way to make sure nothing falls through the cracks.
Version control is your best friend. When you create an updated chart, the old one must be clearly marked 'ARCHIVED' and immediately taken out of active use. This simple step prevents anyone from accidentally using an outdated and potentially dangerous document.
Archiving and Version Control
Managing different versions of the chart is a huge part of the process. One of the most common and dangerous mistakes is leaving old charts lying around. Imagine a support worker grabbing a chart from last month that doesn’t list a newly prescribed blood thinner—the risk is enormous.
A simple system for version control is non-negotiable. Every version of the NDIS medication chart should have a clear date on it, like "Version: 15 October 2025". When you make an update, the new chart gets a new date, and the old one is formally archived.
Whether you're using a digital system or a physical binder, having a strict protocol for retiring old documents is essential for safe support. Proper management of these records often falls under core tasks funded by different NDIS support categories, which really highlights how central it is to a participant’s overall plan.
Common Questions About NDIS Medication Charts
Even with a perfect system on paper, the day-to-day reality of managing an NDIS medication chart brings up real-world questions and the occasional tricky situation. Knowing the answers ahead of time helps everyone—participants, families, and support workers—handle these moments with confidence.
Let's face it, using a medication chart is more than just ticking boxes. It’s about navigating the nuances and having a clear plan for all those "what if" scenarios that inevitably pop up.
Handling Mistakes on the Chart
We’re all human, and mistakes can happen. What really matters for safety and compliance is how you correct them. If a support worker makes an error on a paper chart, the protocol is straightforward and non-negotiable.
You should never use white-out or scribble over the mistake until it's unreadable. The correct method is to draw a single, neat line through the incorrect entry, ensuring it can still be read. Right next to it, write the correct information, then add your initials and the date of the correction. This method keeps the record transparent and honest.
Crucially, any error, no matter how small it seems, must be reported to a supervisor straight away. This almost always means filling out an incident report, following the provider's specific policy. When it comes to a participant's safety and keeping an accurate NDIS medication chart, transparency is everything.
Managing PRN or 'As Needed' Medications
PRN, or "as needed," medications demand special attention because they aren't on a fixed schedule. To prevent any confusion or misuse, they must have their own clearly marked section on the chart.
This section needs to detail:
- The medication's name (e.g., paracetamol).
- The specific reason for its use (e.g., for headache relief).
- The minimum time required between doses (e.g., wait at least 4 hours).
- The maximum number of doses allowed in a 24-hour period.
Every single time a PRN dose is given, the support worker has to log the exact time, the dose administered, their initials, and a quick note explaining why it was needed. This detailed log is vital for preventing accidental overdoses and gives the GP valuable information during medication reviews.
Using Digital Apps for NDIS Records
A common question we hear is whether a digital app can officially replace a traditional paper chart. The short answer is yes, but with a big "if"—it must meet the strict NDIS requirements for safety, accuracy, and detailed record-keeping.
A compliant app must create an unchangeable audit trail, showing exactly who gave what medication and when. It also needs a secure place for notes and has to be easily accessible to everyone on the authorised team. Before you even think about switching, make sure the app is secure, reliable, and that every single staff member is properly trained on how to use it. It's always a good idea to double-check that your provider’s policies officially approve digital records.
Who is Responsible for Chart Updates
While one person might be in charge of physically writing on the chart, keeping it accurate is a shared responsibility. Think of it as a team effort between the participant, their family or advocate, their support workers, and their healthcare providers.
Any change from a doctor—a new medication, a different dosage, or stopping a medication altogether—must be updated on the chart immediately. This has to happen before the next dose is due. Everyone on the team has a role to play in flagging when an update is needed.
This collaborative mindset is a huge part of person-centred care. It’s built on the same principles as a strength-based approach, which is all about empowering people by focusing on their capabilities and support networks. You can learn more about what is a strength-based approach in our related guide.
At Vana Care, we believe clear communication and rock-solid processes are the bedrock of outstanding disability support. If you're in Adelaide or regional South Australia and need a provider who puts safety, consistency, and genuine connection first, we're here to help. Find out more at https://www.vanacare.com.au.


