Your Guide to NDIS Mental Health Support

Navigating the world of NDIS support for mental health can feel a bit like learning a new language. At its heart, though, it’s about practical, real-world help for your day-to-day life. The official term you'll hear is psychosocial support, and it’s essentially a personalised toolkit designed to help you manage the challenges a mental health condition creates. The focus is squarely on your independence and goals, not just on clinical treatment.
What Is NDIS Mental Health Support, Really?
Let's cut through the jargon. When people talk about "NDIS mental health support," they're almost always referring to funding for a psychosocial disability. This isn't about treating your diagnosis—that's the role of the clinical health system, which includes your GP, psychiatrist, or hospital. Instead, the NDIS steps in to address the functional impact your condition has on your daily life.
Here's an analogy that might help. Imagine someone has arthritis. A doctor prescribes medication to manage the pain—that's the clinical treatment. The NDIS, on the other hand, might fund grab rails in the bathroom or a ramp for the front door to help them move around their home safely. It's the same principle for mental health. A psychologist provides therapy (clinical), while an NDIS-funded support worker might help you create a manageable daily routine, get to your appointments, or rediscover a hobby you’ve drifted away from.
Shifting the Focus to Practical Recovery
The real difference is the mindset. NDIS psychosocial support is all about building your capacity to live the life you want, on your own terms. It’s a partnership focused on helping you achieve your personal goals, whatever they might be. This could mean learning new skills for managing the household, finding the confidence to join a local group, or even exploring volunteer or work opportunities.
The aim is to move beyond simply managing symptoms. It's about empowering you to actively participate in your community and regain a sense of control over your own life. It’s about building resilience and personal sovereignty.
This kind of support is deeply personal and flexible. It acknowledges that recovery isn't a straight line and your needs will likely change over time. The NDIS funds supports that help in very tangible ways.
For instance, your plan might include funding for:
- A recovery coach: Often someone with their own lived experience of mental health challenges, they can guide you through the system and help you stay on track with your recovery goals.
- A support worker: A hands-on helper who can assist with daily tasks, from grocery shopping and meal planning to providing transport and support at social events.
- Therapeutic supports: This could include seeing an occupational therapist to develop practical skills and strategies for everyday living.
To help you get comfortable with the language of the NDIS, here’s a quick breakdown of the core concepts you’ll come across.
Core NDIS Psychosocial Concepts at a Glance
This table demystifies the key terms in NDIS mental health support and explains what they mean for your journey.
| Concept | What It Means for You |
|---|---|
| Psychosocial Disability | This is the official term for when a mental health condition significantly impacts your ability to manage daily life, connect with others, or work. It’s the ‘why’ behind your NDIS funding. |
| Functional Impact | This refers to the specific, practical ways your condition affects you. For example, it might make it hard to concentrate, maintain relationships, or leave the house. Your NDIS plan is built around addressing these impacts. |
| Capacity Building | This is about funding supports that help you learn new skills and become more independent over time. Think of it as an investment in your long-term well-being, not just a short-term fix. |
| Recovery Coach | A specialist support coordinator with lived or learned experience of mental health recovery. They are your guide, helping you understand your plan and connect with the right supports to achieve your goals. |
Ultimately, NDIS psychosocial support is there to bridge the gap between clinical treatment and real-world living. It provides the scaffolding you need to build skills, connect with your community, and pursue a life that is meaningful to you.
How to Know If You Are Eligible for Support
Figuring out if you qualify for NDIS mental health support can often feel like the toughest part of the journey. The secret is to understand what the NDIS is actually looking for. It's less about your specific diagnosis and more about the real-world functional impact of your mental health condition—what the NDIS calls a psychosocial disability.
Think of it this way. Having a diagnosis is like having a recipe for a cake. But the NDIS needs to know if you have the ingredients and tools to actually bake it. They want to see how your condition creates significant, ongoing barriers that stop you from participating in everyday life.
Essentially, the NDIS needs proof that your disability is both permanent and has a substantial impact on your ability to function. "Permanent" doesn't mean you'll never have good days or that recovery isn't possible. It just means the condition is likely lifelong, even if the intensity of its effects fluctuates.
Proving Your Disability Is Permanent and Substantial
To get your application across the line, you need to collect evidence that tells a clear story about your life. This goes beyond just a medical report; it’s about showing how your diagnosis translates into day-to-day challenges.
The NDIS will look closely at how your condition affects your capacity in a few key areas:
- Social Interaction: Do you struggle to make or keep friends, feel overwhelmed in social settings, or find it hard to understand social cues?
- Self-Care: Are there challenges with personal hygiene, remembering to take medication, or preparing your own meals?
- Self-Management: Is it tough to plan your day, organise tasks, make decisions, or manage your emotions?
- Mobility: Does anxiety or a lack of motivation make it difficult to even leave the house?
- Communication: Do you have trouble expressing what you need or understanding what others are telling you?
- Learning: Do you face problems with concentration, memory, or picking up new skills?
The trick is to use concrete examples. Instead of just saying, "I have social anxiety," you could explain, "My anxiety is so severe that I can't use public transport, which means I can't get to appointments or see friends on my own."
Key Takeaway: It’s all about cause and effect. Your application needs to connect the dots for the NDIS, showing exactly how the consequences of your mental health condition limit your independence and stop you from being part of your community.
Gathering the Right Evidence
A successful application is built on solid proof. You'll need to gather documents from different professionals who know you and your situation well. The most important piece of the puzzle is usually a detailed report from your psychiatrist, psychologist, or another qualified practitioner.
This report needs to do more than just name your diagnosis. It should spell out the functional impacts it has on your life. It’s a great idea to work with your practitioner on this, making sure they describe not just the clinical symptoms but how those symptoms create the daily struggles we listed above. If you're looking for a wider view of the support systems out there, you might find our guide on navigating NDIS in Adelaide helpful.
Even with a clear need, many people hit roadblocks. The numbers show that the percentage of NDIS participants with a primary psychosocial disability is lower than it should be. Only 10.4% of participants are in this category, falling short of the 13.9% forecast. This gap suggests that many people who are likely eligible are struggling with the application process, which really highlights why building a clear, well-supported case is so critical. You can dig deeper into these findings in this Mental Health Australia report.
What Kind of Help You Can Actually Get

So, your NDIS plan has been approved. Now for the important part: turning that plan into real, practical help that makes a difference in your day-to-day life. The world of NDIS mental health support is vast, but it's not just a grab-bag of services. Think of it more like a toolkit, filled with supports designed to help you build a more stable, connected, and fulfilling life, one piece at a time.
The support you receive is always tied back to your personal goals and the specific ways your psychosocial disability impacts your life. It’s all about practical assistance that helps you manage your daily activities and connect with your community in ways that are genuinely meaningful to you. The system is set up to deliver help where you need it most.
Building Your Daily Routines and Skills
A huge part of NDIS funding often goes toward creating structure and fostering independence at home. When symptoms like low motivation, overwhelming anxiety, or deep fatigue make everyday tasks feel like climbing a mountain, the right support can be a game-changer.
For example, your plan could fund:
- A support worker to help you with grocery shopping and preparing meals, so you always have nutritious food available.
- An occupational therapist to help you design morning and evening routines that reduce stress and feel manageable.
- Help with household chores that have become too much, freeing up your mental energy for recovery.
Sometimes, the most powerful changes come from improving the fundamentals. For instance, good sleep is absolutely essential for mental wellness. You might find that looking into expert-backed strategies for deep rest can be a fantastic complement to your formal NDIS supports.
Connecting with Your Community
Social isolation can be one of the toughest parts of living with a psychosocial disability. NDIS support can act as a bridge, helping you reconnect with the world around you at your own pace and in a way that feels comfortable and safe.
This could look like:
- Having a support worker go with you to a local art class, a community garden, or the gym.
- Funding for a therapist who specialises in social skills, helping you practise conversations in real-life situations.
- Support to attend community events or join groups that match your hobbies and passions.
Key Idea: The goal isn’t just about getting you out of the house. It's about nurturing genuine connections and a sense of belonging, which are vital for long-term mental wellbeing.
These supports exist because mental illness is a leading cause of disability in Australia. In fact, as of December 2021, over 53,000 NDIS participants listed a psychosocial disability as their primary condition, showing just how significant this area of support is. This specialised NDIS mental health support helps people overcome the very real barriers they face in social settings, communication, and daily life.
Finding Meaningful Work or Activities
Having a sense of purpose is a powerful part of any recovery journey. The NDIS can fund supports that help you explore work or volunteer roles that align with your strengths and interests.
This might involve a specialist consultant helping you with your resume and interview practice, or a support worker assisting with transport to get you to a volunteer position. The specific combination of services you get will be laid out in your service agreement. If you're new to this, our guide to your NDIS service agreement is a great place to start to understand exactly what you're entitled to.
A Step-by-Step Guide to Your NDIS Application
Applying for NDIS mental health support can feel like a mountain to climb, but you don’t have to do it alone. Let's walk through it together. Think of this as your practical roadmap, breaking the whole process down into clear, manageable steps. With the right preparation, you can put together an application that truly reflects your needs.
The journey starts with gathering the right evidence. This isn't just about getting a quick letter from your doctor; it's about painting a complete picture of how your psychosocial disability impacts your day-to-day life. Every report and statement should work together to tell a consistent and powerful story.
Your Application Checklist
To build a strong application, you’ll need a solid foundation of evidence. Start by gathering these key documents:
- Evidence of Diagnosis: This is the formal document from a qualified health professional that confirms your mental health condition.
- Medical and Treatment History: Gather reports from your GP, psychiatrist, or psychologist. These should outline your treatment journey so far.
- Functional Impact Reports: This is absolutely crucial. Ask your occupational therapist or psychologist for a report that details exactly how your condition affects your daily functioning in areas like self-care, social interaction, and communication.
- Personal Statements: A letter from you, in your own words, explaining your goals and the challenges you face is invaluable. Statements from carers or family members who see your struggles firsthand can also add significant weight to your application.
The image below gives you a bird's-eye view of the entire journey, from that first assessment right through to getting your supports in place. It really helps to visualise the path ahead.
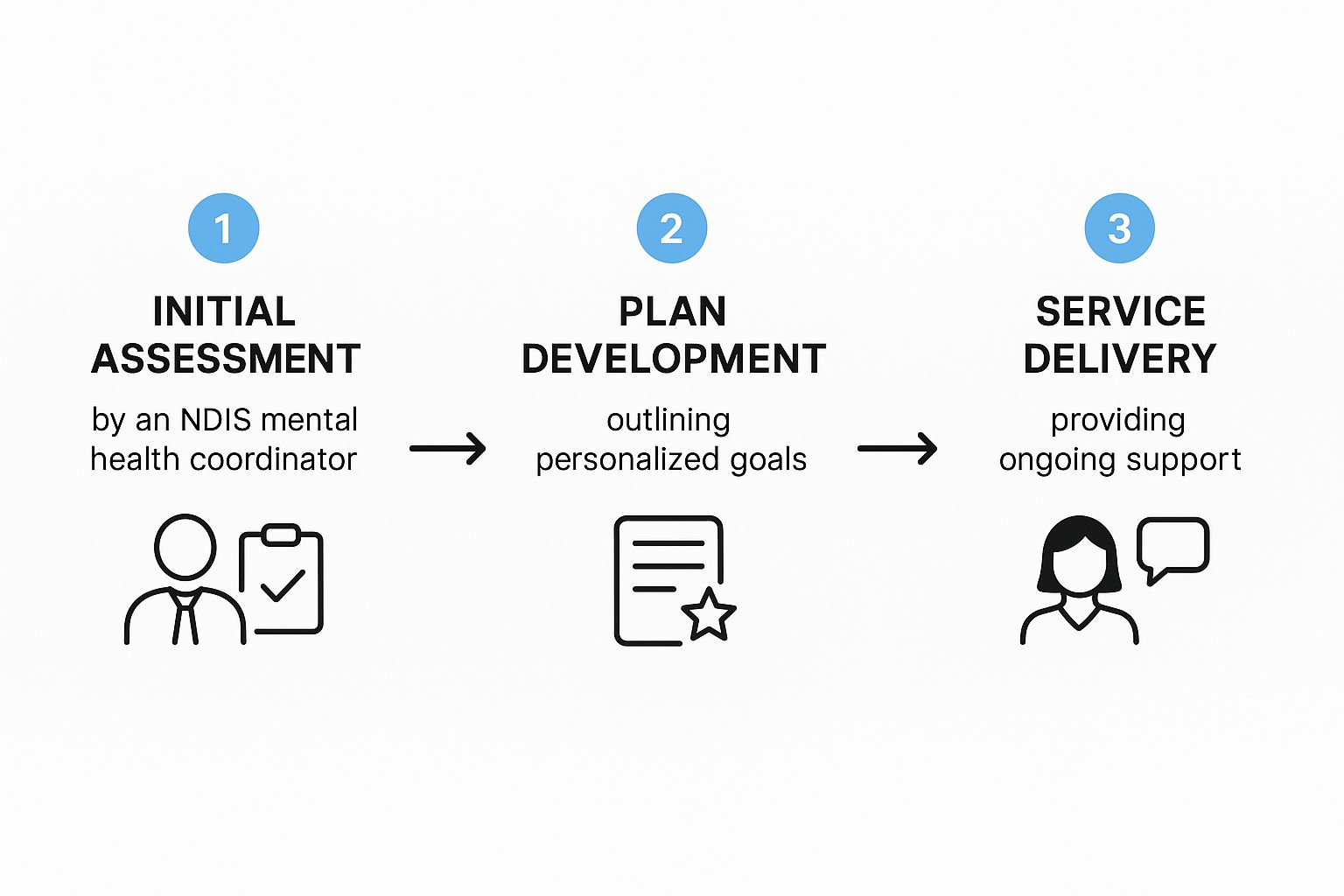
As you can see, once your application is assessed, the focus shifts to creating a personalised plan. Only then can your services actually begin.
Telling Your Story Effectively
Once your documents are in order, the next step is filling out the Access Request Form and getting ready for your planning meeting. This is your opportunity to connect every support you're asking for directly to your disability and what you want to achieve in life.
Be specific. Use real-world examples. Instead of just saying, "I need help with cooking," explain why. Try something like: "Because of my low energy and difficulty concentrating, I often skip meals or end up with unhealthy takeaways. A support worker could help me plan, shop for, and prepare simple, nutritious meals a few times a week." See the difference?
Key Tip: For every challenge you bring up, link it to a personal goal. For instance, "My social anxiety makes it incredibly hard to leave the house (that's the challenge), but I really want to join a local art class to feel more connected to my community (that's the goal)." This simple framing shows the NDIS exactly how their funding will help you build your skills and independence.
Knowing how to prepare for your NDIS plan and its future reviews is a critical skill. To get you ready for these important conversations, we’ve put together a complete insider's guide on achieving NDIS plan review success. Getting your plan right from the very beginning makes everything that follows so much smoother.
What to Do If Your Application Is Unsuccessful

It can feel like a punch to the gut when your NDIS application is rejected. After all the time and emotional energy you’ve poured into it, it's natural to feel disheartened or even a bit lost. But this isn't the end of the road. Think of it less as a "no" and more as a "not yet."
If the NDIA decides you’re not eligible, you have the right to ask for an internal review. This is your first and most important next step. It means a different person at the NDIA—someone who wasn't involved in the first decision—will take a completely fresh look at your application and all the evidence you submitted. It’s like getting a second opinion from a new specialist.
Building a Stronger Case for Review
This review is your chance to address the reasons your application was knocked back. Go back to the decision letter and pinpoint exactly where the NDIA felt the information was lacking. This is your roadmap for strengthening your case.
Here are a few things to consider:
- Gather more specific evidence: Could an occupational therapist provide a more detailed functional assessment that clearly outlines your day-to-day challenges?
- Seek updated reports: Ask your GP, psychiatrist, or psychologist for a new report. This time, make sure it explicitly connects your diagnosis to the specific ways it impacts your ability to function independently.
- Polish your personal statement: Read through your statement again. Does it paint a clear picture of your goals and how NDIS funding is the key to helping you achieve them?
Your goal is to leave no doubt in the reviewer's mind about how your psychosocial disability creates real barriers in your life. Don't be afraid to be specific and detailed—connect the dots for them.
An unsuccessful application is often not a final rejection of your need for support. Instead, it’s usually a signal that the NDIA needs a clearer, more complete picture of your situation. The review process is your opportunity to provide just that.
Looking Beyond the NDIS
It's also really important to know that the NDIS isn't the only game in town. Australia has a whole network of mental health support systems, and there are fantastic options available even if an internal review doesn't go your way. Many people find exactly what they need through other government-funded or community-based mental health services.
The reality is, there's a significant gap between the number of people who need psychosocial support and what the NDIS can provide. In 2019-20, for example, it was estimated that around 290,000 Australians with severe mental illness needed this kind of help. Only about 34,000 received it through an NDIS plan, while another 75,000 were supported by other government programs. This just goes to show how vital these alternative services are. You can read the full government analysis of psychosocial support needs to understand the bigger picture.
Many of these services focus on building practical life skills and fostering social connections. Our guide on community access support services is a great starting point for finding valuable local programs. At the end of the day, the goal is getting the right support for you, no matter which door it comes through.
Common Questions About NDIS Mental Health Support
When you start digging into NDIS mental health support, it's natural for a lot of practical questions to pop up. Getting straight answers is the first step to feeling confident about your choices. Let's walk through some of the things people ask most often.
One of the biggest sources of confusion? It’s all about who pays for what. It’s a completely fair question and a really important one.
Can the NDIS Pay for My Psychologist or Psychiatrist?
This is a really common point of confusion, so let's clear it up. The short answer is no, not usually. The NDIS doesn’t fund services that are considered part of the mainstream clinical health system.
Psychiatrists (who diagnose and prescribe medication) and psychologists (who provide clinical treatments like CBT) are covered by Medicare and the health system. That's their territory.
Where the NDIS steps in is with funding for therapeutic supports that focus on capacity building. Think of it this way: it’s less about clinical treatment and more about improving your skills to navigate daily life. So, while Medicare might cover your psychologist sessions to treat a mental health condition, your NDIS plan could fund an occupational therapist to help you build practical strategies for managing social anxiety when you're shopping or catching public transport.
It's about gaining real-world skills, not just receiving clinical therapy.
Support Coordinator vs. Recovery Coach: What Is the Difference?
At first glance, these two roles might seem similar, and they can sometimes overlap. But a Support Coordinator and a Recovery Coach bring very different kinds of help to the table. Knowing which is which helps you get the right guide for your journey.
-
Support Coordinator: Think of them as your NDIS logistics expert. Their main job is to help you understand and use your plan. They’ll connect you with providers, help you sort out service agreements, and generally make sure you’re getting the most value out of your funding. They are your guide to the NDIS system itself.
-
Recovery Coach: This is a much more specialised role within NDIS mental health support. A Recovery Coach almost always has their own lived experience with mental health challenges, which is invaluable. They work alongside you, your family, and your other supports to design a life that you find meaningful, focusing on your personal recovery, resilience, and goals.
Key Insight: A Support Coordinator is the 'how-to' person for your plan. A Recovery Coach is focused on your 'why'—why these supports are important for your personal recovery and what you want for your future.
How Do I Prepare for My NDIS Plan Review?
Your plan review is a crucial moment. It’s your chance to share what’s been working, what hasn’t, and to make the case for the support you'll need over the next year. The key is not to leave it to the last minute.
Start gathering your evidence well in advance. Pull together reports from your support workers, therapists, and your recovery coach. These reports should paint a clear picture of the goals you’ve been working on, the skills you’ve gained, and the barriers you’re still facing. Keeping a simple log of how you've used your current funding can also be incredibly helpful. For more ideas on this, check out these expert support strategies for in-home care for disabled individuals, as they offer great insights into documenting your needs effectively.
Go into your meeting ready to talk about your goals for the next 12 months. Be specific about the supports you think will help you get there. The more clearly you can connect a requested support to one of your personal goals, the stronger your request will be.
At Vana Care, we know that genuine connection and consistent, reliable support make all the difference. Our team is here to walk with you through every step of your NDIS journey, offering compassion and expertise. Learn more about our personalised disability support services at https://www.vanacare.com.au.


