A Guide to Positive Behaviour Support NDIS

When you hear the term Positive Behaviour Support, or PBS, what comes to mind? It’s more than just managing difficult situations. At its heart, Positive Behaviour Support is a deeply respectful and evidence-based way of understanding why someone might be using certain behaviours to communicate what they need. It’s about looking past the action itself to discover the message behind it.
Under the National Disability Insurance Scheme (NDIS), PBS is a key approach to improving a person's quality of life and reducing behaviours that might be causing concern for them or others.
What Is Positive Behaviour Support Within The NDIS?

Navigating the NDIS can feel like learning a new language, with countless terms and acronyms. But Positive Behaviour Support really stands out. It represents a fundamental shift in thinking—moving away from simply reacting to a person's challenging actions and towards proactively supporting their overall wellbeing and understanding their unmet needs.
Think of it this way. If a plant is wilting, you don't just paint the leaves green to make it look healthy. A good gardener gets to the root of the problem. Is it getting enough water? Is the soil right? Does it need more sunlight? In the same way, a Positive Behaviour Support practitioner looks for the root cause of a behaviour to create real, lasting change.
The Core Idea: Behaviour Is Communication
Every behaviour, no matter how it looks on the surface, is a form of communication. When someone can't easily express their wants, frustrations, or needs through words, they might use actions instead. These actions can sometimes be misunderstood or seen as 'challenging'.
A PBS plan is all about teaching new, more effective ways to communicate and get those needs met.
The ultimate goal of a PBS plan is to ensure the person with a disability is supported safely and in a person-centred manner that addresses their wants and needs to improve their quality of life.
This isn’t about a quick fix or discipline. It's a thoughtful, collaborative journey that involves creating supportive environments, building positive relationships, and empowering the individual. The NDIS funds PBS through the 'Capacity Building' budget because it does just that—it builds a person's skills and strengthens the ability of their entire support network to help them thrive.
What A Positive Behaviour Support Plan Involves
A successful PBS strategy isn't a single action but a blend of several key elements that work in harmony. It’s a holistic approach that considers the whole person—their skills, their relationships, and their environment.
Here’s what you’ll always find at the core of a good PBS plan:
- Getting to the 'Why': Practitioners carry out detailed assessments to figure out the function of a behaviour. What is the person trying to achieve or communicate?
- Building New Skills: The plan focuses on actively teaching new skills—like communication, social interaction, or emotional regulation—that achieve the same outcome in a more effective way.
- Creating a Better Environment: This involves making practical changes to a person’s surroundings to reduce triggers and make daily life more predictable and supportive.
- A Team Approach: It's not just about the participant. The plan provides essential training and guidance for family, carers, and support workers so that everyone is on the same page, applying the strategies consistently and confidently.
This multi-layered approach helps create sustainable, long-term improvements in a person’s independence and community connection. It lays the groundwork for a more fulfilling life, one built on a foundation of understanding and empowerment, not control.
What Are the Goals of a Positive Behaviour Support Plan?
A Positive Behaviour Support (PBS) plan is much more than a document—it’s a living, breathing roadmap designed to make a real difference in a person’s life. The main goal is always to improve their quality of life, creating clear paths toward greater happiness, independence, and a stronger connection to their community.
Ultimately, we want to reduce and, ideally, eliminate the need for restrictive practices altogether. This is done by getting to the root cause of a behaviour, rather than just reacting to the symptoms we see on the surface. It’s a fundamental shift from being reactive to being proactive. Instead of just managing difficult moments as they happen, a good PBS plan helps everyone anticipate a person's needs and build an environment where they feel safe, heard, and ready to take on life's challenges.
Teaching New Skills for Better Communication
One of the most powerful parts of Positive Behaviour Support is its focus on building new skills. The plan helps us figure out what a person is trying to communicate through their actions and then teaches them a more effective way to express that same need.
Think about someone who gets really distressed in noisy places. The behaviour we see might be yelling, which is their way of saying, "This is overwhelming!" A PBS plan doesn't just try to stop the yelling. It digs deeper and teaches a replacement skill. This could look like:
- Learning to use a communication card that says, "Quiet, please."
- Practising a simple hand signal to show they need a break.
- Getting comfortable asking for headphones before going into a loud space.
These new skills are empowering. They give the individual a sense of control and a much more direct way to get their needs met, which in turn reduces distress and builds genuine confidence.
The aim is to make the new, positive skill a more efficient and effective way of communicating than the old behaviour ever was. When that happens, the behaviour of concern often just becomes unnecessary.
Creating Supportive and Proactive Environments
A person’s surroundings play a massive role in their wellbeing. A huge part of any PBS plan is shaping the environments at home, at school, and out in the community to be more supportive and less stressful. This isn’t about wrapping someone in cotton wool; it’s about making smart, practical adjustments to head off common triggers before they cause a problem.
For someone who finds comfort in predictability, some simple environmental strategies might include:
- Visual Schedules: Using pictures or a simple list to show what the day’s activities look like.
- Consistent Routines: Making sure daily tasks happen in a familiar and expected order.
- Sensory Adjustments: Things like dimming bright lights or using noise-cancelling headphones for someone with sensory sensitivities.
By making these kinds of changes, the entire support network becomes proactive. This stability eases anxiety and frees up the person’s mental and emotional energy to focus on learning, growing, and enjoying life.
At its heart, a core objective of any Positive Behaviour Support plan is to build a person's independence by developing essential Autism Life Skills. This focus on practical, real-world abilities is key. By helping someone become more independent, participate in their community, and build meaningful relationships, a PBS plan funded through the NDIS doesn't just manage behaviour—it opens up a world of new possibilities.
How To Access PBS In Your NDIS Plan
Getting funding for positive behaviour support in your NDIS plan can feel a bit daunting, but it’s absolutely doable if you’re well-prepared. The real secret is showing exactly how PBS will help you or your loved one build new skills and chase those personal goals. It's less about just "managing" challenges and more about unlocking potential.
This journey actually starts well before you walk into your NDIS planning meeting. Your first mission is to gather solid, relevant evidence that tells a clear story about the need for specialist behaviour support. Don't think of it as focusing on the negatives; think of it as highlighting where the right kind of support can make a world of difference.
Building Your Case With The Right Evidence
Imagine you're a detective building a case for support. Your job is to give your NDIS planner or Local Area Coordinator (LAC) all the information they need to see why positive behaviour support ndis funding is both reasonable and necessary.
Your evidence needs to connect the dots. It should clearly show how certain behaviours are linked to a person's disability and how they're acting as roadblocks to achieving important life goals, like getting involved in the community, forming friendships, or living more independently.
Here’s the kind of paperwork that really strengthens your case:
- Reports from Allied Health Professionals: Think assessments from occupational therapists, speech pathologists, or psychologists. These often pinpoint challenges with communication, sensory needs, or emotional regulation that are key to understanding behaviour.
- School or Day Program Reports: Notes from teachers or support workers can be invaluable. They often describe specific incidents, what might have triggered them, and the effect on learning and socialising.
- Medical Letters: A letter from a GP or specialist can explain the underlying diagnosis and officially link it to the need for behaviour support.
- Your Own Records: Never underestimate the power of your own observations. A simple diary or logbook where you’ve noted down challenging situations, what was going on at the time, and what happened next provides authentic, real-world insight.
The more organised and compelling your evidence is, the smoother your conversation will be when it comes time for your planning meeting.
Aligning PBS With Your NDIS Funding
It's helpful to know where PBS fits into the NDIS framework. Positive Behaviour Support is funded under the Capacity Building support category, specifically falling under the budget for Improved Daily Living. Knowing this helps you speak the right language.
How you frame your request really matters. You’re not just asking for funds to "stop" a behaviour. What you're actually asking for are the resources to build life-changing skills that lead to a better quality of life.
When talking about your needs, always bring it back to the goals. Explain how PBS will help the participant learn new ways to communicate, develop better coping skills, and ultimately gain more independence and be more involved in their community.
It’s also important to remember that behaviour support and physical health are often intertwined. People who need behaviour support often have complex health needs too. In fact, data shows NDIS participants who access PBS services tend to use medical services more than the general population. This just goes to show how vital it is to have a well-rounded behaviour support plan that considers a person's overall health.
Preparing For Your Planning Meeting
Once you have your evidence file ready, you can advocate with confidence. In your planning meeting, be direct and clear that you are requesting funding for a Functional Behaviour Assessment (FBA) and the creation of a Positive Behaviour Support Plan.
Use your evidence to back up what you're saying. For instance, you could say, "As you'll see in this report from his school, my son's issues with loud, busy places mean he misses out on things like school assemblies. We believe a PBS plan could teach him strategies to handle that sensory overload."
After your plan is approved, the next step is to find a provider. A key part of this is putting a service agreement in place, which details the support you'll receive. Taking the time to understand what goes into a good agreement is smart, as it protects your rights and ensures you get the most out of your funding. For a detailed guide on this, check out our guide on NDIS service agreements. It will help you formalise things with your chosen PBS practitioner and move forward with peace of mind.
Choosing A Qualified NDIS Behaviour Support Practitioner
Finding the right person to guide your positive behaviour support NDIS journey is one of the most critical decisions you'll make. This isn't just about ticking a box or hiring a service; it's about building a genuine partnership founded on trust, shared understanding, and real human connection. A great practitioner does far more than just write a plan—they listen deeply, collaborate openly, and empower everyone involved to move forward together.
The professional you choose becomes an integral part of the support network. That's why it’s so important to find someone who not only holds the right qualifications but also builds a strong, respectful rapport with the NDIS participant and their family. This connection is the bedrock on which lasting, positive change is built.
Understanding Practitioner Qualifications
To ensure you're in safe and capable hands, the NDIS Quality and Safeguards Commission has set up a clear framework for behaviour support practitioners. This system gives you peace of mind, knowing that the professional you work with meets national standards for skill, safety, and ethics.
It's not a one-size-fits-all qualification. Instead, it's a tiered system that acknowledges different levels of experience and expertise, making sure practitioners have the right skills for the complexity of support needed.
The levels are:
- Core: Practitioners at this level can conduct assessments and develop straightforward plans, usually working under supervision.
- Proficient: These are experienced professionals who can work more independently across a broader range of situations.
- Advanced: Highly skilled practitioners capable of managing complex cases and providing supervision and mentorship to others.
- Specialist: True experts in the field, often leading complex cases and contributing to research, policy, and sector development.
This system creates a high bar for professionals delivering positive behaviour support NDIS services. The oversight is surprisingly strict. For instance, in 2022, while 8,715 practitioners were initially deemed suitable, only 2,529 had been formally approved after a rigorous assessment of their skills and evidence. If you’re interested in the data, you can learn about the NDIS practitioner framework findings.
Questions to Ask a Potential Practitioner
When you meet with a potential practitioner, it helps to have some questions ready. This is your opportunity to get a real feel for their approach, their experience, and how they would work with your family.
Your goal is to find a practitioner whose professional style aligns with your family’s values and the participant's personality. The right fit makes all the difference in achieving meaningful, long-term change.
Here’s a checklist of key questions to get the conversation started:
- What is your experience working with people with similar needs and goals? This question helps you understand if they have relevant expertise and truly grasp the unique challenges you're facing.
- How do you involve the participant and their family in developing the plan? A great answer will focus on collaboration, listening, and keeping the participant at the very centre of every decision.
- Can you walk me through your process for a Functional Behaviour Assessment? A good practitioner should be able to explain their methods for observing and gathering information in a way that’s clear and makes sense to you.
- How will you train and support our family and other support workers to implement the plan? The most effective plans are the ones everyone feels confident and equipped to carry out day-to-day.
- How do you measure success and what does progress look like to you? Their answer should be about improving quality of life, building new skills, and reducing distress—not just stopping a behaviour.
Making this choice is a huge step in any NDIS journey. If you’re looking at your options here in South Australia, it’s also useful to know what makes any disability provider a great one. For more practical advice, feel free to read our Vana Care guide on choosing the right disability support in Adelaide.
The PBS Process: From Assessment to Implementation
Embarking on a Positive Behaviour Support (PBS) journey can feel like a big step, but it’s a well-structured and collaborative process that unfolds in clear, manageable stages. It's not about quick fixes; it's about getting to the root of things. The whole process is a genuine partnership between the participant, their family, and the practitioner.
It all starts with a deep dive to understand the individual. From there, a tailored plan is carefully put together, followed by ongoing support and fine-tuning. This isn't a one-and-done deal, but a continuous cycle of learning and adapting to ensure the strategies stay relevant and effective as the person's needs evolve.
Stage 1: The Functional Behaviour Assessment
The very first step is the Functional Behaviour Assessment, or FBA. Think of this as the discovery phase. The behaviour support practitioner essentially becomes a detective, gathering clues to understand the 'why' behind a particular behaviour. They don't just look at the behaviour in isolation; they investigate the entire context surrounding it.
This isn't some formal test in a sterile office. It's a real-world, collaborative effort to gather information, which usually involves:
- Direct Observation: The practitioner spends time with the person in their natural environments—at home, out in the community, or at a day program. This gives them a firsthand look at what daily life is really like.
- Interviews: They'll chat with the key people in the person's life, from family members and support workers to teachers. These conversations are gold, offering invaluable history and insight into the person's strengths, preferences, and challenges.
- Data Collection: The team might track when behaviours happen to spot patterns. Does it occur around a certain time of day? In a specific place? When a particular request is made?
The whole point of the FBA is to develop a clear theory—a hypothesis—about the function of the behaviour. What is the person trying to achieve or communicate? Are they seeking connection, trying to escape a stressful situation, wanting something specific, or perhaps responding to sensory overload? Answering this question lays the groundwork for everything that comes next.
Stage 2: Designing the Behaviour Support Plan
Once the FBA is done and we have a good handle on the 'why', the practitioner works closely with the support network to create the Positive Behaviour Support Plan (PBSP). This isn't a generic template pulled off a shelf; it's a highly personalised document built around the individual's specific goals, strengths, and needs.
A quality plan, funded through the positive behaviour support NDIS framework, is much more than a list of "don'ts." It's a proactive roadmap focused on what everyone should do to help the person succeed.
A great PBSP gives the entire support team practical tools. It shifts the focus from just reacting to problems to proactively building an environment where the person feels understood, safe, and supported to flourish.
The plan will detail several key elements:
- Proactive Strategies: These are all about making changes to the environment or routines to head off triggers before they happen, reducing the chances of the behaviour occurring in the first place.
- Skill-Building Goals: This is the heart of the plan. It spells out the new skills the person will be taught—like new ways to communicate their needs or handle big emotions—that achieve the same outcome as the old behaviour.
- Reactive Strategies: The plan also provides clear, safe, and consistent steps on how to respond if the behaviour of concern does happen, with de-escalation and safety always being the top priorities.
This journey is best seen as a continuous loop.
The infographic below shows the three core stages of the Positive Behaviour Support process, from figuring out the needs right through to ongoing review.
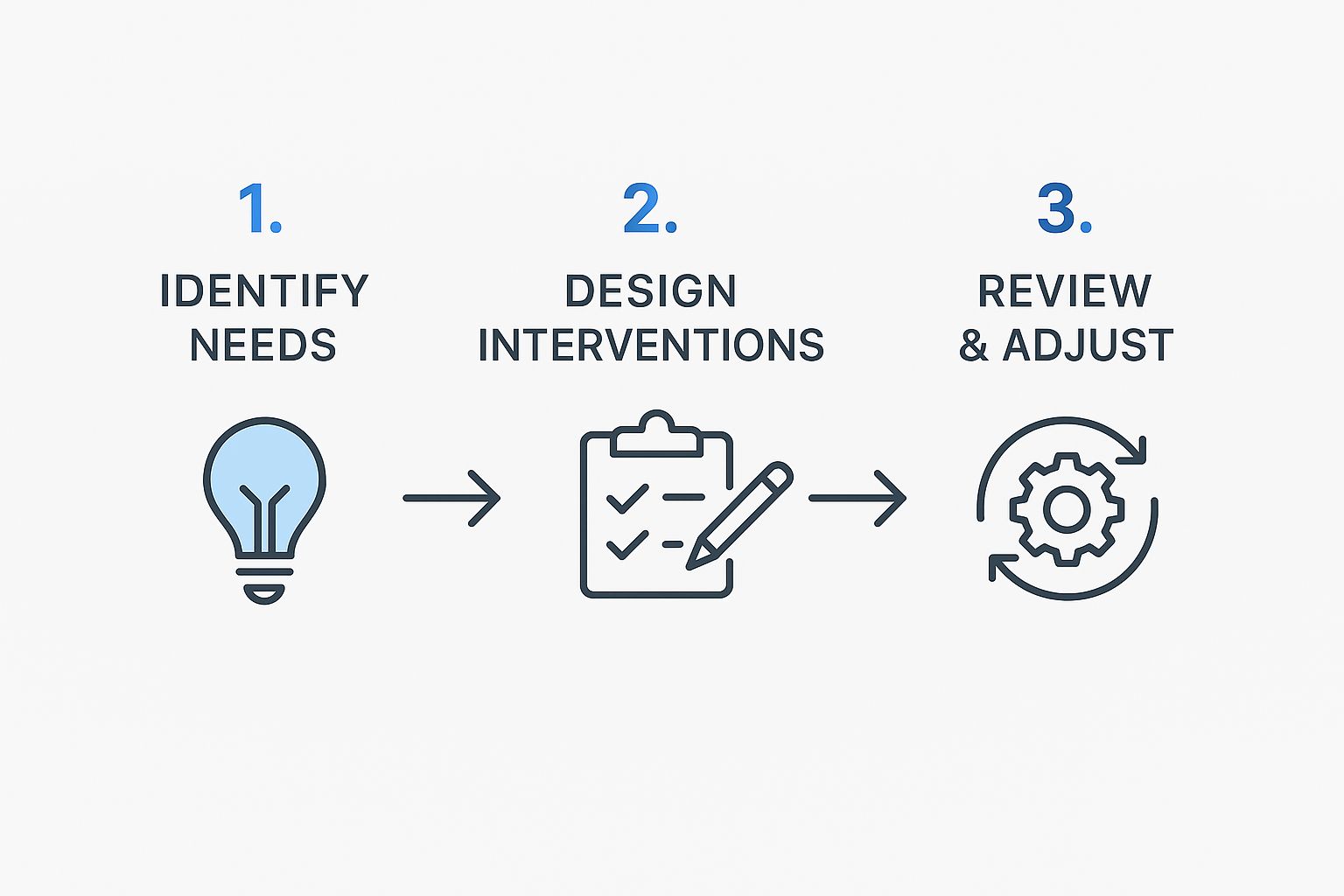
This visual really drives home that PBS isn’t a straight line with a finish line. It’s a constant cycle of improvement and adjustment.
Stage 3: Implementation and Ongoing Review
A plan is only as good as its execution. This final stage is all about putting the strategies into action, which means proper training and coaching for everyone involved. The practitioner will work side-by-side with family and support workers to make sure they feel confident and ready to use the plan consistently.
From there, it’s all about monitoring and reviewing. The team checks in regularly to see what’s landing well and what might need a tweak. Is the person picking up the new skills? Are the proactive strategies making a real difference?
Life changes, and as the participant grows, so must the plan. This ongoing review process ensures the support stays effective and keeps enhancing the person's quality of life, which is central to the future of disability care trends and innovations.
Navigating Common Challenges In PBS Delivery

While the ideas behind Positive Behaviour Support are powerful and clear, putting them into practice isn't always a straight road. It’s important to be honest about the hurdles you might face—not to get discouraged, but to be ready to tackle them head-on. Knowing what to expect is the first step to finding a way through.
It’s a common experience for families and practitioners to find themselves navigating service systems that can feel clunky or slow. Trying to get everyone on the same page—from schools and therapists to support workers—can sometimes feel like a full-time job in itself, even when everyone is doing their best.
These aren't just one-off stories. A significant survey of behaviour support practitioners across Australia recently highlighted this exact problem. The study pointed to real-world barriers in delivering quality positive behaviour support NDIS services, like system hold-ups and struggles with getting everyone to work together. If you're interested in the details, you can explore the full study on barriers and enablers in PBS delivery.
Fostering a Supportive Ecosystem
The same research that laid out the challenges also pointed to the solutions. The best results happen when there's strong organisational support, excellent practitioner supervision, and a real commitment to ongoing training. Simply put, a well-supported practitioner is a much more effective one.
Think of it like a sports team. A star player can only achieve so much alone. To truly succeed, they need a great coach (supervision), a solid game plan (organisational support), and plenty of practice (training). When a provider invests in these key areas, the quality of care for the NDIS participant skyrockets.
The resilience of a PBS plan lies not just in the document itself, but in the strength and alignment of the entire support network surrounding the individual.
This is where clear and consistent communication becomes your most valuable asset. Setting up a simple communication system, like a shared digital document or a quick weekly email update, can make sure everyone from the teacher to the support worker is working from the same playbook.
Proactive Strategies For Success
Instead of just reacting to problems as they pop up, you can build a more resilient support network from the very beginning. By thinking ahead about common roadblocks, you can create a much smoother and more effective positive behaviour support NDIS experience.
Here are a few proactive strategies that can make a huge difference:
- Schedule Regular Team Meetings: Carve out a consistent, short time for all the key people to connect. Even a quick 30-minute virtual catch-up every couple of weeks can prevent small misunderstandings from becoming big problems.
- Define Roles and Responsibilities Clearly: Right from the start, make sure everyone knows exactly what their role is. Who’s the main contact for school issues? Who’s responsible for tracking progress on a new skill? This clarity stops important tasks from falling through the cracks.
- Invest in Quality Training: Ensure that all support workers get direct training from the behaviour support practitioner. This gives them the confidence and practical skills they need to apply the strategies consistently and correctly.
Ultimately, getting through these challenges is all about building a strong, collaborative team that's focused on the same goal. Real success is born from a sense of shared purpose and mutual support, which is a core part of our vision for community empowerment through disability support. By working together with clear communication, you can turn potential hurdles into stepping stones for genuine growth.
Your NDIS Behaviour Support Questions, Answered
When you're looking into positive behaviour support NDIS funding, it’s completely normal to have a few questions. Let's walk through some of the most common things we get asked by participants and families across South Australia, breaking down the answers in a clear and simple way.
How Long Does PBS Take to Work?
There's no magic number here. Because Positive Behaviour Support (PBS) is tailored to the individual, the timeframe for seeing results can vary quite a bit. Some people start showing positive shifts in just a few weeks. For others with more complex support needs, it might be a journey of several months or even longer.
The real measure of success isn't speed; it's about making steady, lasting progress. It all comes down to how consistently the strategies are used and whether everyone in the support network is truly on board. We're focused on building foundational skills that improve quality of life for the long haul, not just finding a temporary fix.
What Is the Difference Between a Practitioner and a Psychologist?
This is a great question, as their roles can seem similar. Think of it this way: a psychologist is a registered health professional who can diagnose and treat mental health conditions. Their expertise is broad and often clinical.
A behaviour support practitioner, however, has a very specific focus. They are specialists in conducting what's called a Functional Behaviour Assessment (FBA) and then designing a PBS plan to address particular behaviours of concern. While some psychologists are also qualified practitioners, the roles are distinct. Practitioners must meet a specific NDIS capability framework that centres on applied behaviour analysis and person-centred support.
A core goal of Positive Behaviour Support is to reduce and, wherever possible, eliminate the need for restrictive practices. The entire focus is on proactive, positive strategies first.
Will a PBS Plan Use Restrictive Practices?
A PBS plan will only include what’s called a 'regulated restrictive practice' as an absolute last resort. This is reserved for situations where there is a serious and immediate risk of harm to the person or those around them.
Any time a restrictive practice is considered, it is heavily scrutinised and regulated by the NDIS Quality and Safeguards Commission. It has to be documented in detail, formally approved, and—most importantly—be part of a clear strategy to phase it out. This is done by teaching the person safer, more effective ways to communicate their needs. The end goal is always to increase a person's freedom and quality of life.
Understanding how PBS contributes to your bigger picture is vital. You can explore how it aligns with your broader goals in our guide to the NDIS capacity building framework. This helps connect the dots on how different supports can work together to build true independence.
At Vana Care, we believe in building strong, supportive partnerships to help you achieve your goals. If you're looking for a provider in Adelaide or regional South Australia who puts genuine connection first, get in touch with us to see how we can help. Learn more at https://www.vanacare.com.au.


