What Is Community Nursing? Discover Its Key Roles & Benefits

So, what is community nursing? At its heart, it’s a special kind of nursing that breaks free from the hospital walls. Instead of you travelling to a clinic or hospital, the nurse comes to you—whether that’s in your own home, at a local health centre, or even at school.
Understanding Community Nursing Beyond Hospital Walls
Think of a community nurse as a 'mobile health hub' dedicated to you. Their job isn't just about patching up an illness and moving on. It’s about understanding the whole person—your life, your environment, and the personal factors that shape your health. It’s about delivering care that genuinely fits you.
This approach is a shift from simply reacting to sickness. Instead, it’s about proactively helping people manage their health right where they live. The focus is on giving individuals the tools and confidence they need to live as safely and independently as possible. This could mean anything from showing someone how to manage their diabetes to providing complex wound care at home, often preventing a disruptive hospital stay.
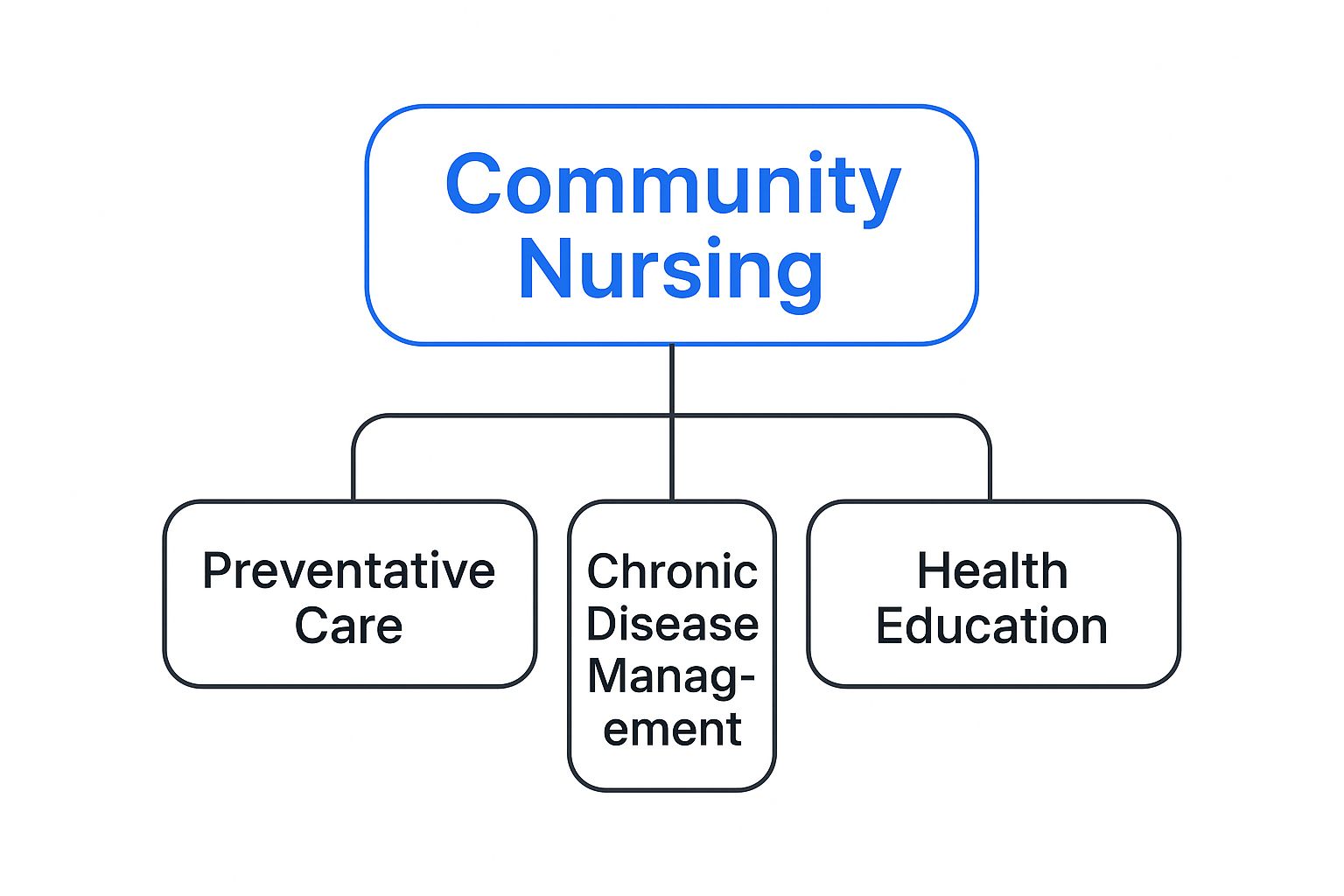
As you can see, the role is a dynamic mix of preventative care, managing long-term conditions, and providing essential health education—all delivered right in the heart of the community.
A Holistic And Proactive Approach
The foundational principle of community nursing is holistic care. This means looking beyond a list of symptoms on a chart and seeing the entire person. By building real relationships and getting to know someone’s unique situation, community nurses can coordinate much more effective and meaningful support. It’s a person-first philosophy that truly fosters community empowerment through disability support.
This way of delivering healthcare is becoming more critical every year. With Australia's population getting older, the need for accessible, home-based services is growing fast. In fact, projections show that by 2057, nearly 1 in 4 Australians will be aged 65 or over. This demographic shift puts a huge emphasis on finding smart, community-based solutions to meet our nation's health needs.
To really grasp the difference, it helps to see the two nursing models side-by-side. This table breaks down the core distinctions between working in the community versus a hospital.
Community Nursing vs Hospital Nursing at a Glance
| Aspect | Community Nursing | Hospital Nursing |
|---|---|---|
| Work Environment | Patient's home, schools, clinics, community centres. Highly variable. | Structured hospital or clinical setting. Controlled environment. |
| Patient Relationship | Long-term, ongoing relationships built on trust and familiarity. | Short-term, episodic care focused on a specific illness or injury. |
| Focus of Care | Health promotion, disease prevention, chronic condition management. | Acute care, diagnosis, treatment of immediate health crises. |
| Autonomy Level | High degree of independence and autonomous decision-making. | Works within a larger, hierarchical team structure with direct supervision. |
| Scope of Practice | Broad and holistic, considering social, family, and environmental factors. | Narrow and specialised, focusing on the specific medical condition. |
| Goal | To promote independence, self-management, and quality of life at home. | To stabilise the patient, treat the acute issue, and discharge them. |
Looking at this comparison, you can see how community nursing isn’t just hospital care moved to a different location—it’s a fundamentally different approach to health and wellbeing.
The Changing Face of Community Nursing in Australia

If you picture community nursing as just basic home visits from decades past, it's time for a new image. The reality today is a highly specialised and dynamic field of healthcare, constantly evolving to meet the changing needs of Australian society. It’s no longer just about who needs care, but how that care is best delivered well beyond the hospital walls.
Two major forces are behind this shift: our ageing population and the growing number of people living with chronic health conditions. As more Australians live longer, many are managing complex illnesses like diabetes, heart disease, or respiratory conditions at home. This has created a huge demand for expert, ongoing nursing support right where people are most comfortable.
Adapting to Modern Healthcare Demands
Meeting these challenges head-on means today's community nurses have a much broader skill set. A physical visit is just one part of the job. A modern community nurse might conduct a follow-up consult via telehealth, coordinate a complex care plan involving multiple specialists, and seamlessly blend medical treatments with crucial social support services.
This evolution is absolutely vital for our entire healthcare system. By managing conditions effectively in the community, these nurses are on the front line of preventing unnecessary and costly hospital stays. This not only gives people a better quality of life but also takes immense pressure off our busy hospitals.
Community nurses are at the forefront of a systemic shift, moving the focus from acute, reactive treatment in hospitals to proactive, preventative care delivered directly in the community. Their work is essential for building a more sustainable and person-centred healthcare future.
Addressing Critical Workforce Pressures
This expanded role has also put a spotlight on the significant pressures facing our healthcare workforce. The skills needed for effective community nursing—things like clinical autonomy, holistic assessment, and sharp problem-solving in unpredictable home environments—are incredibly specialised. The problem is, the demand for these professionals is growing much faster than we can supply them.
This isn't just a minor issue; it's a national concern. Government projections are sounding the alarm, signalling a potential shortage of 85,000 nurses by 2025. If things don't change, that number could swell to 123,000 by 2030. This shortfall hits community care particularly hard, where the need for experienced, independent practitioners is most critical. You can explore the full workforce report to see the data behind these projections.
All of this makes the role of the community nurse more vital than ever before. They are an indispensable link in Australia’s healthcare chain, holding the system together one home visit at a time.
A Day in the Life of a Community Nurse

To really get a feel for community nursing, you have to picture a day that unfolds not within the walls of a hospital, but across suburbs and living rooms. Forget the predictable rhythm of ward rounds; this is a role defined by its variety, autonomy, and the unique challenges that come with every new front door.
A community nurse’s day doesn't start with a formal handover in a sterile staff room. It usually begins at home, with a cup of coffee and a careful review of the day's schedule. They’ll be checking patient files, mapping out the most efficient route between appointments, and methodically packing the car with everything they might need—from complex wound dressings to specific medications.
The Morning Appointments
The first stop might be at the home of an older gentleman who is just back from the hospital after major surgery. Here, the nurse’s skills are on full display. They're not just changing a dressing; they’re conducting a thorough clinical assessment, managing his pain relief, and expertly creating a sterile field on a coffee table. It's about adapting hospital-grade care to a home environment.
Next, it’s a short drive to see a young adult managing Type 1 diabetes. This visit is less about hands-on treatment and more about education and empowerment. The nurse will review blood glucose logs, talk through dietary choices, and maybe help troubleshoot a new insulin pump. The goal is to build the person's confidence and skills for effective self-management.
A community nurse's car is so much more than just a vehicle. It's a mobile office, a supply cupboard, and the very thing that enables them to meet people exactly where they are.
Afternoon Care and Coordination
After a quick lunch on the go, the afternoon could shift to a palliative care visit. These appointments call for a profound level of compassion and expert communication. The nurse focuses on providing comfort, managing symptoms, and offering a steadying presence for both the patient and their family. It’s about preserving dignity and enhancing quality of life.
Later, the nurse might be supporting an NDIS participant. This work goes beyond clinical tasks. It's about enabling independence and fostering greater https://vanacare.com.au/blogs/vana-care-blog-ndis-news-disability-support-insights-for-south-australia/community-participation-ndis. By managing their health needs at home, the nurse is helping them build the capacity to get out, engage with others, and chase their personal goals.
The day typically winds down with a block of crucial admin time. This isn’t just paperwork; it’s the backbone of good care.
- Updating Patient Records: Meticulously documenting every visit, observation, and conversation.
- Coordinating with Other Professionals: Liaising with GPs, physiotherapists, and support coordinators to ensure a seamless, team-based approach.
- Planning for Tomorrow: Looking ahead to the next day’s appointments and anticipating what each person will need.
This constant juggling of autonomous work and collaborative communication is what makes the role so dynamic. For a closer look at the sheer breadth of tasks involved, it's worth understanding in more detail what a home care nurse does, as their daily duties are incredibly diverse.
Ultimately, a day in the life of a community nurse is a powerful display of clinical expertise, adaptability, and genuine human connection. They are the problem-solvers, educators, and trusted advocates who make it possible for so many Australians to live safely and independently at home.
How Community Nursing Supports NDIS Participants
The National Disability Insurance Scheme (NDIS) is built on a simple but powerful idea: giving people with disabilities genuine choice and control over their lives. Community nursing fits into this picture perfectly. It acts as a vital bridge, allowing NDIS participants with more complex health needs to live safely and independently in their own homes, not in a hospital or clinical setting.
For so many participants, community nursing is the key that unlocks a new level of freedom. It goes way beyond standard personal care, delivering specialised, high-intensity support that can only be provided by a qualified nurse. This is where you see the real impact of community nursing within the NDIS—it’s about managing serious health conditions in a way that helps people live their life, rather than restricting it.
Delivering High-Intensity NDIS Supports at Home
So, what do these high-intensity supports actually look like day-to-day? They are very specific, often complex tasks that are absolutely critical for a person's health and can't be done by a regular support worker. A community nurse, funded through an NDIS plan, brings this clinical expertise right to your doorstep.
The NDIS recognises that some health needs require a registered or enrolled nurse. Here's a table outlining some of the most common high-intensity supports that can be funded.
| Support Category | Examples of Nursing Tasks | Goal for the Participant |
|---|---|---|
| Complex Bowel Care | Administering suppositories or enemas, digital stimulation. | To manage bowel health with dignity and prevent complications. |
| Ventilator Management | Monitoring equipment, managing settings, suctioning. | To breathe safely and comfortably at home. |
| Tracheostomy Care | Cleaning the site, changing dressings, suctioning the tube. | To keep the airway clear and prevent serious infections. |
| Enteral Feeding | Managing PEG or NG tubes, administering formula, flushing lines. | To receive essential nutrition safely and effectively. |
| Subcutaneous Injections | Administering medications like insulin or blood thinners. | To manage chronic conditions and prevent hospital visits. |
These aren't just medical procedures; they're life-enabling services. When a skilled nurse can manage these needs at home, an NDIS participant can avoid constant, disruptive trips to the hospital and get on with building a full and meaningful life. You can learn more about how this works in our detailed guide to expert in-home care for disabled individuals.
A Person-Centred Partnership
What truly strengthens the link between community nursing and the NDIS is the shared belief in person-centred care. This isn’t about a nurse just ticking off a list of tasks. It’s about building a genuine partnership where the participant is at the heart of every single decision.
A community nurse working with an NDIS participant doesn't just ask, "What medical task do I need to do?" They ask, "How can my skills help you achieve your goals today?"
This collaborative approach is everything. A great community nurse knows they are part of a wider team and works closely with other allied health professionals. For instance, knowing about useful occupational therapy resources can help them create a more holistic support plan that covers all aspects of a person’s independence.
By weaving clinical care together with therapeutic goals, community nurses help transform an NDIS plan from a document into a dynamic tool for building confidence, skills, and real connection—all from the comfort of home.
The Real-World Benefits of At-Home Care

Opting for community nursing is about so much more than just convenience. It’s a choice with powerful, positive ripple effects for individuals, their families, and the entire Australian healthcare system. The most obvious benefit, of course, is the profound comfort of recovering in your own home.
There's something uniquely healing about being surrounded by your own things, your routines, and the people you love. This familiar environment does more than just feel good—it actively reduces stress, which in turn can have a huge impact on mental wellbeing and physical recovery.
We see it time and time again: people often heal faster and have fewer setbacks when they're in a comfortable, low-stress setting. Community nursing makes this a reality by bringing skilled, clinical care right to your doorstep. It’s about delivering that expert medical support without the clinical feel or disruption of a hospital stay.
Empowering People and Their Families
One of the most powerful aspects of community nursing is patient empowerment. It’s not just about doing for people; it’s about working with them. Our nurses take the time to teach crucial skills for managing health at home.
This could mean showing someone how to confidently administer their own medication, manage the day-to-day realities of a chronic condition, or spot the early warning signs of a potential issue.
This focus on education builds a person's confidence and gives them a real sense of control over their health. They stop being a passive recipient of care and become an active, knowledgeable partner in their own wellbeing. Families are brought into this circle of support, too, gaining the skills and reassurance to help their loved one. This collaborative approach is central to person-centred care, and you can learn more about what families should know in our detailed guide.
By bringing care home, community nursing doesn't just treat an illness; it supports a person's entire life, promoting independence and dignity in a way a clinical setting rarely can.
A Smarter, More Sustainable Model for Healthcare
The benefits don't stop at the front door. This model of care has a massive positive impact on the broader healthcare system, making it more efficient and sustainable for everyone. Think about it: every time a community nurse helps someone manage their health safely at home, it prevents a potential hospital admission.
This one act frees up a vital hospital bed for someone facing a genuine, acute emergency. The systemic advantages are clear:
- Fewer Hospital Readmissions: With proactive support and monitoring at home, we can catch and manage small issues before they become big problems that require a trip back to the hospital.
- Safer, Earlier Hospital Discharges: Patients can often leave the hospital sooner when a solid, professional home care plan is ready and waiting for them, ensuring a smooth transition.
- Greater Cost-Effectiveness: It is almost always more cost-effective to support someone in their home than it is to pay for a long and expensive hospital stay, which eases the burden on our public health system.
At its core, community nursing represents a more compassionate, patient-first, and economically sensible way to deliver modern healthcare in Australia.
How to Become a Community Nurse in Australia
If you're feeling drawn to the idea of working more independently and making a real, tangible impact in people's homes, then a career in community nursing might be calling your name. It’s a rewarding path, but one that’s built on a solid foundation of education, practical skill, and a specific set of personal strengths.
The first, non-negotiable step is becoming a Registered Nurse (RN). This journey begins with completing a Bachelor of Nursing at university. This degree gives you the essential clinical knowledge and hands-on skills that form the bedrock of professional nursing practice.
Once you graduate, you’ll need to register with the Australian Health Practitioner Regulation Agency (AHPRA). This registration is your official license to practise legally as an RN anywhere in Australia.
The Makings of a Great Community Nurse
Your degree gets you in the door, but it’s your personal attributes that will make you truly shine as a community nurse. This role is different. You’re working on your own in a person’s private space, which demands a skillset that goes far beyond the hospital ward.
Think of it this way – you need to be:
- Highly Autonomous: You must be comfortable and confident making important clinical decisions on the spot, often without a team standing right behind you.
- A Sharp Critical Thinker: Every home environment is unique. You need the ability to quickly assess complex situations, spot potential risks, and create care plans that actually work in the real world.
- Genuinely Empathetic: Building trust is everything. You need to connect with people on a human level, showing true compassion and understanding as a guest in their home.
These qualities are absolutely vital when you're helping someone achieve greater independence. A community nurse might be the key support for a person transitioning into a new home, a role that’s part clinical expert and part trusted advisor. To see how this plays out in practice, you can explore our guide on what is Supported Independent Living.
A great community nurse doesn’t just bring healthcare into a home; they bring confidence, reassurance, and a clear plan for empowerment, adapting their approach to fit each person’s unique life and goals.
After you’re qualified and registered, the doors open to a wide variety of opportunities. You could find yourself working for a government-run local health district, a not-for-profit organisation, or a private agency focused on specialised in-home care.
This variety means you can find the perfect fit for your career goals, launching a truly fulfilling career right in the heart of your community.
Your Questions Answered
It's completely normal to have questions when you're exploring healthcare options. Let's walk through some of the common ones about community nursing to help you see how it all fits together.
What’s the Difference Between a Community Nurse and a Support Worker?
Think of it like this: the main difference comes down to their training and the specific kind of support they can give you.
A community nurse is a qualified professional—either a Registered or Enrolled Nurse—who handles the clinical side of your care. This includes medical tasks like giving injections, managing complex wounds, or looking after a tracheostomy.
A support worker, on the other hand, is your go-to for essential, non-clinical help. They're the ones who can assist with personal care, preparing meals, or keeping your home tidy. Both roles are incredibly important for living well at home, but only a nurse is qualified to perform medical procedures.
Do I Need a Referral to Get a Community Nurse?
Yes, a referral is usually the first step. This isn't just a piece of paper; it’s the official handover from your doctor or hospital that ensures your community nurse has all the right information from day one.
Typically, the referral will come from your GP, the discharge team at the hospital, or another health specialist who knows your case. If you're an NDIS participant, your support coordinator can also be a huge help in getting the ball rolling, especially if nursing support is included in your plan.
Think of the referral as the bridge between your different care providers. It ensures the nursing team has the correct medical background to give you safe, effective, and personalised care right from the start.
How Is Community Nursing Paid For in Australia?
Funding for community nursing in Australia isn't a one-size-fits-all situation. It can come from a few different places, depending on your individual circumstances:
- Government Health Services: State and territory governments fund a lot of community nursing, usually through your local health district.
- The NDIS: If you're an NDIS participant, the scheme can fund high-intensity nursing supports that are directly linked to your disability.
- Private Health Insurance: Some private health policies include cover for nursing at home, which is often used for support after a hospital stay.
- Paying Privately: You always have the option to self-fund private community nursing services directly.
At Vana Care, our passion is matching NDIS participants with skilled and genuinely caring community nurses. We're here to help you live more confidently and independently in your own home. To see how our person-centred approach can help you achieve your health goals, take a look at our NDIS nursing services.


